Telemedicine and technology are crucial ways to deliver care and keep our health care workers, patients and vulnerable populations safe, especially amid the COVID-19 pandemic. This discussion is designed to share best practices and the latest policy and payment updates to support physicians and practices in expediting the implementation of telemedicine. This conversation should also outline the ways in which technology and telemedicine can strengthen physician/patient relationships, even in trying times like those of the current COVID-19 pandemic, so care can continue to be provided to those who need it most.
Communication during this time of crisis is critical. TranslateLive's award winning software was just made temporarily free ($500 value) for anyone to use with no signup, email or questions asked. Please see video for more details. youtu.be/xdfR-dr3Ty0


Plug and Play is hosting a series of COVID-19 webinars highlighting the top startups across different industries that have existing technology solutions that can be quickly implemented and that have specific COVID-19 use cases. Check out the recorded sessions from our last two sessions with our partners at BARDA (Division of the U.S. Department of Health & Human Services) and Roche Diagnostics here: plugandplaytechcenter.com/covi...
As a 3rd-year medical student who is almost finished with his clerkships, what resources are available to get us involved? I've experience with doing phone check-ups and managing chronic conditions amidst this COVID-19 pandemic for our schools free health clinics.
I want to know about opportunities that will expand and utilize the plethora of skills medical students like me have accumulated thus far.
Any ideas, opportunities and resources i can delve into?
Hi Harsh,
PIN Collaborator, Sling Health is discussing some of the clinical problems that are made even more evident by the stress of COVID-19. Tagging Mario, Aadit, Marcus below.
innovationmatch.ama-assn.org/g...
MD++ is also a great group of med students particularly interested in digital health. They are based in New York and I'm tagging their leader Sherman for you as well!
Best,
Great question, future Dr. Patel.
The Texas Medical Association has created a resource page for our physicians. texmed.org/Telemedicine/
Lots of great content to browse and even several forms and policies ready to be put into place.
As has been discussed in this PIN, COVID-19 has dramatically and quite appropriately accelerated the momentum to enable telemedicine. One important dynamic is the growth in physicians providing telemedicine services. Not surprisingly, we are learning that telemedicine requires a complementary, but somewhat new, set of skills. Which is why I am thrilled to see a 3rd year medical student like you interested, since it is not too early to learn.
Hey Harsh!
Thanks for posting. There are so many ways to contribute to healthcare even if you can't get in the clinic currently. A highlight of mine is bringing awareness to the problems currently facing healthcare providers and patients, and then contributing your expertise to help solve these problems. If you've identified problems, you can engage with discussion around that problem at the Clinical Problem Database: innovationmatch.ama-assn.org/g.... Highlighting anything that could use some broader discussion, brainstorming, and solving is very valuable! Furthermore, your clinical background and experience is crucial in developing healthcare solutions sensitive to the experiences of providers and patients. You can work to solve problems by engaging with Sling Health (slinghealth.org) and potentially also getting involved with our COVID19 bootcamp being hosted in May (slinghealth.org/bootcamp).
Thank you so much for your thoughtful answers, I have definitely found opportunities and am looking forward to connecting with like-minded individuals in this coming weeks!
Stay positive, curious and healthy:)
At the forefront of AI technology, IatroCom® built STATworkUP®, an innovative diagnostic medical app for mobile smartphones. The software program runs on the latest iPhone, iPad & Android devices. It is one of the very best medical apps on the market, providing fast problem-oriented information to enable a new era in healthcare delivery. This modern tool was created, over many years, to help improve clinical practice. From the start it was designed to assist healthcare providers do complete evaluation and assessment of concerns. It supports a new approach to patient encounters by caregivers. Doctors, and nurses tell us they love it.
STATworkUP is really a very good value and quite beneficial to own! It quickly correlates symptoms, suggests appropriate lab tests, rapidly integrates findings, and instantly computes differential diagnoses for consideration. The app associates pertinent criteria for over 3,000 conditions to facilitate treatment decisions. It offers fast best-practice guidelines. And it links to related subject matter expert web pages for everything in its large, comprehensive knowledge structure that contains over 12,000 topics plus standard names and synonyms. It includes disease descriptions, etiologies, epidemiology, manifestations, risk factors, causes, complications, remedies, indications, contraindications, adversities, side-effects, interactions and more
Read more about it here:
See it in action here:
You can get the latest version of STATworkUP now, to improve comprehensive examinations, and enhance excellent care:
apps.apple.com/us/app/statwork...
play.google.com/store/apps/det...
When we started Telehealth a few weeks ago we were told to apply POS 2 and modifier -95 to these visits, see "Special coding advice..." from AMA.
Now I have heard we are to use POS 11!
Here is the link to the current "Special coding advice..." from AMA which was updated April 3: ama-assn.org/system/files/2020....
Please help, I don't have much hair left to pull out of my head! If this has changed they cannot be doing this to physician practices that are teetering as it is!
Thank you,
Chris
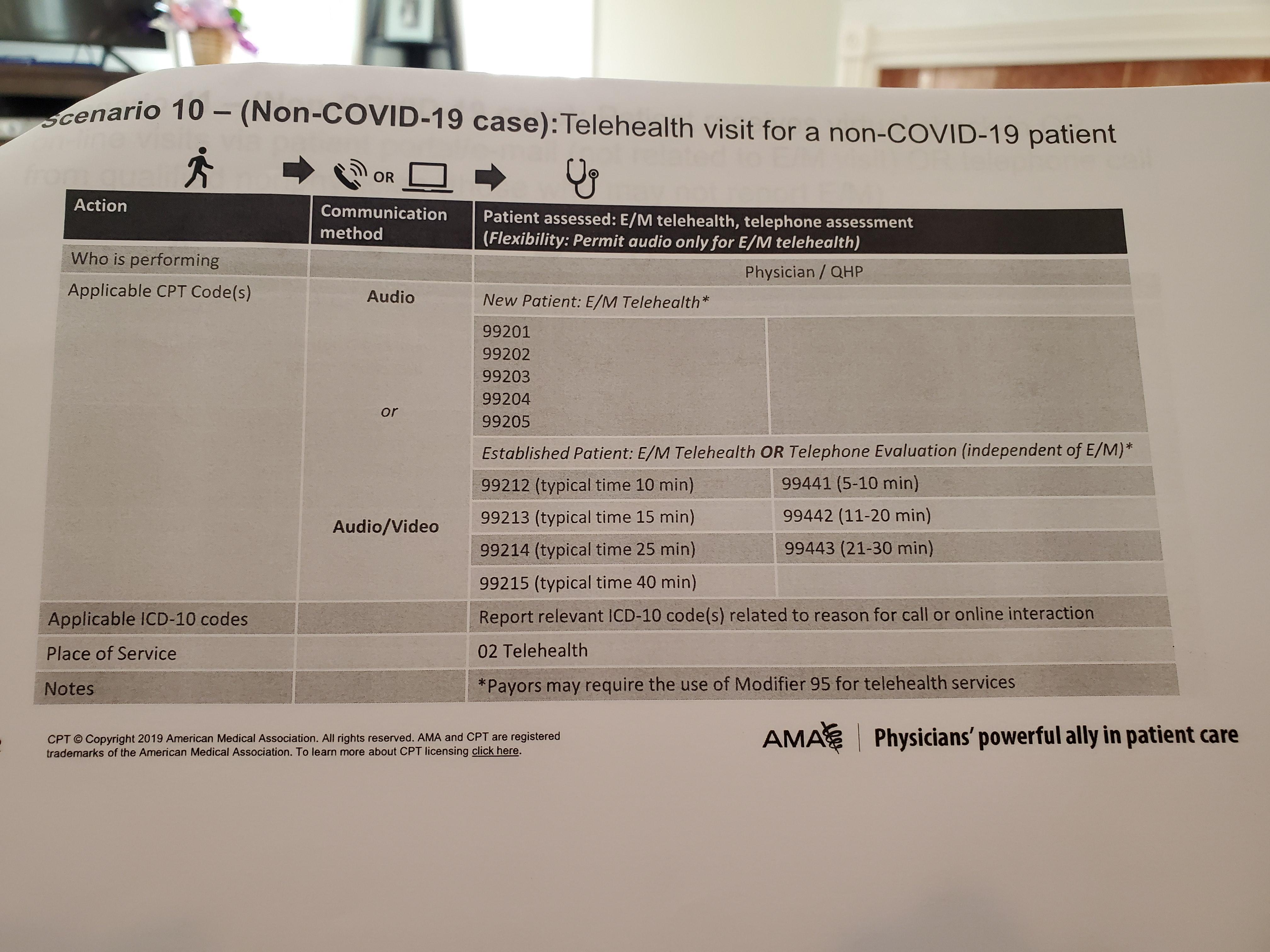
CMS released new guidance last week. In this guidance, CMS asked that the Place of Service (POS) be selected based on where the physician would have otherwise performed the service. For office visits, that would typically be POS - 11, Physician Office. Modifier 95 would be appended to the claim to signal that the service was performs via telehealth This will be to your benefit as this is the mechanism to allow Medicare to pay at the in-person rate. Claims submitted with POS 02 will be paid at the facility rate. CMS also changed the effective date to March 1, 2020.
Thank you for your help. It is so frustrating to have them change this in the middle. It is going to be difficult enough for private practices to make it through this without having to pour energy into these issues
I concur 100% with Dr. Garofalo. I can only imagine the tremendous effort, resources correcting and/or adjusting for billing changes to correct previously submitted CMS invoices. This disruption is ill-timed when we need to concentrate all our resources to save lives for not only this current pandemic but also for the next COVID-19 outbreak.
The frustration expressed is understandable. But, thank you to the AMA for identifying a shortcoming and helping CMS take steps to remedy it for the long term betterment of physicians.
Let's all keep our eyes open for other changes we can make to serve patients in this trying time.
Dr. Silva, do not get me wrong. I am thankful to AMA for helping out on this and it does improve our revenue. I guess from a long-term perspective it kind of demonstrates just how silly our billing system is in the 1st place, doesn't it? First you have to figure the E/M code, then add the POS, then add a modifier. There is no need to be this complex, unless the goal is to complicate payments to the ones who are doing the work. I am a Delegate to the AMA so I know the good work they do, but this is the time to truly reevaluate the amount of complexity and layers that have been added over the years. Thank you.
Great points, Dr. Garofalo. Indeed, we see payment systems which have evolved in parallel over decades adding incremental layers of complexity along the way. For a time, it looked like MACRA would prompt the move from fee for service to broader bundled episodes of care. But, even that has been slow moving.
Which is why we all need to keep up the good fight!
Each Payer has their own requirement for POS and Modifier and these are changing regularly as they adapt to the new environment as well. We started tracking these changes in a google spreadsheet for plans nationwide. happy to share that here. rebrand.ly/a3ubaba
First- God bless all of you at the front line serving your country!
Second- I am sorry to hear about the reduction in patient volume and the uncertain future of thousands of doctors clinics. It is so hard to hear the impact of COVID-19 on you, your staff and patients.
Third (the question)- Are doctors that have shifted to a large percentage of their encounters to telehealth, still using their MA's/ NPs for data collection before you begin your encounter? Please share your experiences/ feedback/ suggestions.
I will defer to others on the excellent question Chris poses.
But, I do want to make a comment about patient (beneficiary) consent. The recently released interim-final rule. CMS, to their credit, believes that consent should not interfere with necessary telehealth services. To that end, the annual consent need not be obtained in advance of the telehealth encounter. It may be obtained at the same time. Small change, but helpful.
To lighten the load with in-take our providers have found MayaMD helpful. See MayaMD.ai
Is it not time for the AMA to lead the charge to change the archaic state by state licensing requirements? We know the history of state boards and medical licensing, both good and bad, but surely we can find a way to have national licensing and still achieve local oversight of those actively practicing in a given geographic location. For telemendicine/videomedicine etc to achieve its full potential long term we need to be able to consult across state lines etc and have some form of reimbursement follow for those professional services. This would greatly increase the clinical access and reach of major centers to physicians and patients on a national basis. Thoughts?
From the purely medical point of view, the state boundaries of licensing often create a barrier to delivering the best care. There are issues to resolve: how to interact effectively with state departments of health, comply with state-based medical regulations, and so on-- so a solution is not as straightforward as creating one national licensing application and approval process, or one national "telehealth approval". I'm still in favor of trying to make it work, and resolving the issues, because it will help the patients in need. The benefits of a national solution would seem to outweigh the risks or costs, at least in principle.
Thank you and I fully agree. Any step forward will have issues to be ironed out. Yet, the rapidity of technological change and innovation demands that medicine not lag behind. Just as the training system was revolutionized over a century ago by Halsted, so too must our delivery system be revolutionized to take advantage of the many new innovations for health care delivery. This is particularly true in the case of chronic disease, care followup, multi-specialty consultation etc.
The AMA has longstanding policy supporting state-based licensure. It's important that physicians are licensed where the patient is located to protect the safety of patients, preserve the state or often local standard of care, preserve medical liability laws and a host of other laws and regulations. In short, icensure at the state level is necessary to protect the strong oversight of the practice of medicine and protect the safety of patients. The AMA does strongly encourage and support increased uniformity in requirements for state licensing requirements and the application process, as well as standardization of verification of credentials.
I can see the importance of state-based licensure from the standpoint of laws, liability, and standards. Increasing uniformity would be helpful. If there were a way to facilitate or streamline applications to states that border a clinician's home state, or reduce costs of applying to multiple states, that may help with medical care as well. What comes to mind is "common application" mechanisms that are often used by universities operating as a consortium.
All good points to a degree. First, while it may be longstanding policy of the AMA, that does not mean that the policy should not evolve and change. Second, we already have national standards in place.
For example, final licensing exams upon exit from medical school are national in scope yet only applied within a selective state when an application is filed. Would we suggest that an MD degree from Harvard qualifies that person over an MD degree from Michigan, or Duke? An MD degree is nationally recognized if from any accredited institution.
Again, the various specialty boards have universal qualifying metrics and exams that are given to all qualified candidates. So is some who achieved board certification in a given discipline less certified if that person resided in California versus Ohio? Or because their training program was Johns Hopkins versus Alabama? Board certification is nationally recognized.
This is also true of broader certifications, such as the FACS from the American College of Surgeons which can apply to surgeons from any discipline or any state.
Food for thought I would think.
we have the DEA numbers which are Federal ( I think ) >We could have a federal license to practice all over the country ?
I am very supportive of a national solution. I think the question will be, what is the state's role, and a state's need, in licensing? We have state-based driver's licenses, state-based certifications for a number of things-- presumably because states may have unique and state-specific needs, based on population details, politics, state legislation, and so on. Health-related requirements and departments of health may vary by state. So all of these things would need reconciliation to make a national solution work. I certainly like the idea! The VA is perhaps a role model or example of "how to" in some of these areas, as some of the state-based requirements do not apply there, and this can lead to more seamless and efficient care for both the patients and the system.
Again, all points to be addressed. It makes sense that any physician physically practicing in a locality should be registered with that state board so that if needed, care monitoring can occur. That should also apply in my view, to telemedicine on a national basis as long as a provider in another state registers that he or she is "seeing" patients via tele/video medicine in another particular state. I am sure that someone will raise legal questions regarding interstate commerce. Not sure why that would even apply as we already have interstate commerce on a massive scale.
As far as I know ,one can practice in any VA hospital with any one state license Why not extend this to other health care facilities
Agree. The existing policy on state licensure creates an artificial barrier to expanding patient care that need not exist.
The rule allows a greater range of services which may be provided via telehealth including:
ED visits
Inpatient care
Nursing Visits
Critical Care
Domiciliary Care
Home Visits
Neonatal and Pedi Critical Care
Neonatal Continuing Care
Care Planning for Cognitive Impairment
Psychological and Neuropsychological Testing
PT and OT
Radiation Treatment Management
Social worker, clinical psychologist, speech language pathology services
The Covid-19 related interim final rule released yesterday includes provisions to help physicians care for patients while keeping both parties free from unnecessary exposure.
One of the important updates during the emergency relates to remote patient monitoring. Those services can now be provided to both new and established patients for both acute and chronic conditions. This is an important update.
This could include, say, pulse oximetry monitoring of a Covid-19 positive or suspected patient.
There are quite a few codes to consider, several of which are time-based, such as 99457-8.
Can you clarify the question? Are you asking about changes to policies, practices, needs, or something else?
Thank you, Dr. Weiner for asking.
I was just answering my own question about yesterday's regulatory updates to the remote patient monitoring (RPM) codes. They are now more broadly available for reporting, coding and billing purposes.
But, I would be interested in applications which could enable their clinical use.
Also, to clarify the interim final rule with comment concerns the Medicare program’s payment policy. Please consult the policy of commercial payers and state health programs to ensure that they have the same coverage policy. The organization that I work with — Compassion & Choices — focuses on ensuring access to care for patients with terminal conditions. We have asked most state governors and legislative leaders to ensure coverage and payment parity for telehealth and other virtual care services in state funded healthcare programs and among commercial payers during COVID19.
It's a tool that can be utilized to monitor patients in isolation at home and still get paid for tracking and monitoring COVID 19 and Non Covid 19 Patients.
Good changes relating to RPM, but more to be done. nixonlawgroup.com/nlg-blog/202...
Especially for older patients, many newer technologies are foreign and non-intuitive to them. They need as much simplification as possible with the steps and requirements. Written instructions tend to be a plus. Getting them comfortable with frequent, short, easy, well explained routines is a plus, so that the focus can then be on them as individuals. We also do not need perfection with technologies; we need approaches that are "good enough"-- good enough for effective communication and decisions, without going much further. Another issue is expectations: we need clarity about each person's role, what is expected of them, "do's and don'ts", and the timing.
Great question - continue to check AMA's Telemedicine Quick Guide for best practices that is continually being updated: ama-assn.org/practice-manageme...
Here's some additional recent articles of interest:
hcinnovationgroup.com/covid-19...
wsj-com.cdn.ampproject.org/c/s...
Hi- here is a good but brief report on best practices:
catalyst.nejm.org/doi/full/10....
We are also publishing a paper on telehealth best practices:
Q3014 is the originating site code. Is this billable (and how) if the patient is in a hospital (not rural) and the physician is elsewhere?


